What to Put in a Covid-19 Emergency Home-Care Kit
April 2nd, 2020
Most people who get sick from the coronavirus won’t be going to the hospital. Here’s what doctors say you need to be ready at home.
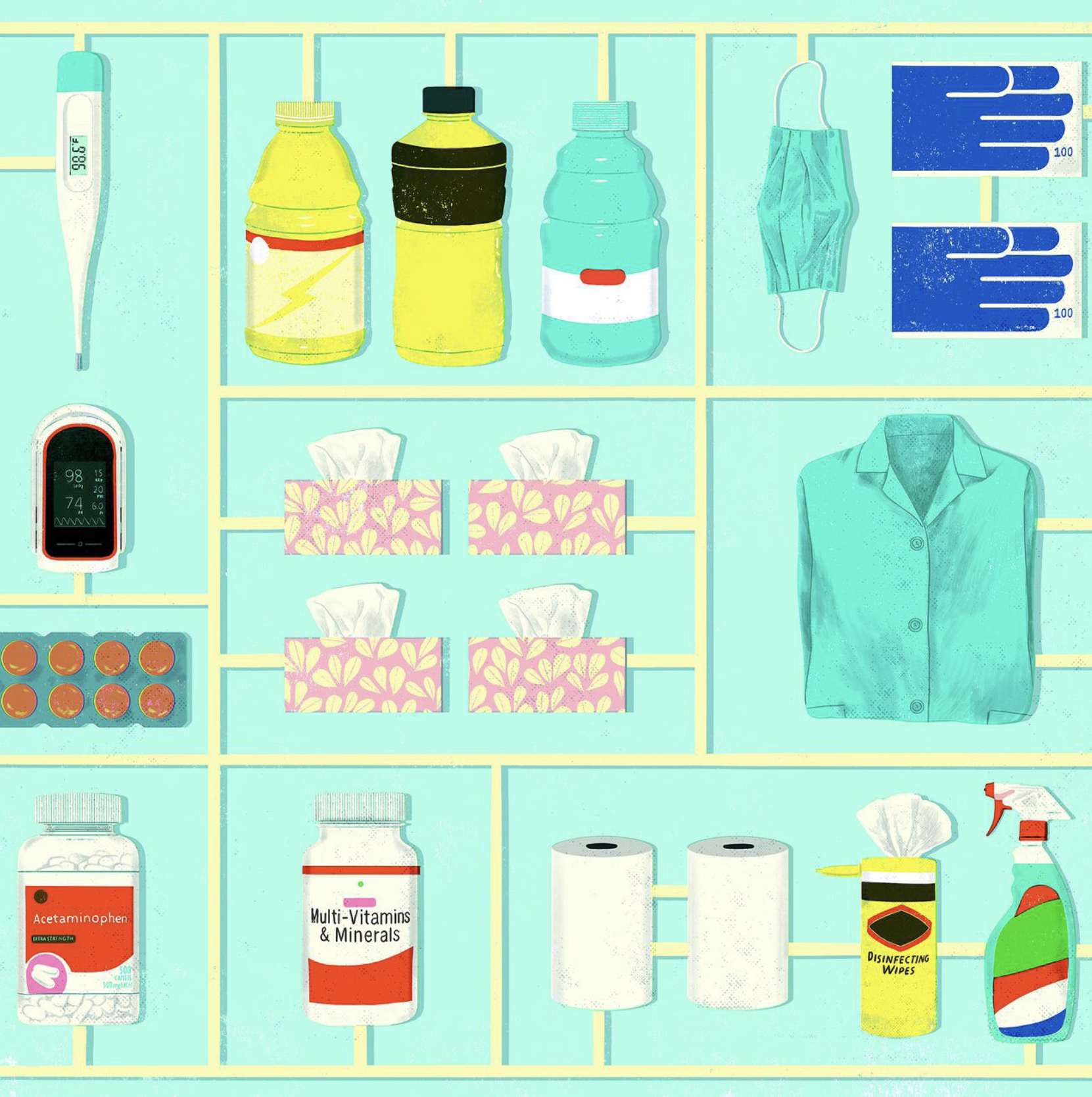
We gathered the best suggestions from doctors at top hospitals all over the country for what to include in their ideal Covid-19 home-care kit. CREDIT: SONIA PULIDO
By Hilary Potkewitz (Wall Street Journal)
If you or a family member gets infected with the coronavirus, it is very likely that you’ll have to ride it out at home.
Most Covid-19 cases don’t require hospitalization, and as intensive-care beds fill, all but the most critical cases are being sent home. So, people should be prepared to care for themselves or their loved ones under their own roof—and that means having the right supplies to nurse the ill patient and keep the rest of the family healthy.
We asked doctors at top hospitals all over the country what they would include in their ideal Covid-19 home-care kit. We gathered their best suggestions and advice to help you organize your own.
SAFETY AND CLEANING
Isolation and cleaning supplies: bleach; face masks that cover nose and mouth (surgical masks, home-improvement masks or scarfs); gloves for entering sick room and doing laundry (latex or nitrile rubber); hand sanitizer; laundry detergent (wash everything on hot); nail brush; paper towels; soap; tissues.
The first task is to isolate patients with their own stash of tissues, disinfecting wipes, paper towels, soap and warm water.
“At the top of my wish list would be an extra bedroom with an attached bathroom. That’s the ideal scenario,” says David Buchholz, senior medical director at Columbia University Irving Medical Center. Most people don’t have that luxury, but it is worth disrupting the rest of the household to try. “If you have a one-bedroom apartment, the sick person gets the bedroom. That’s key. They can’t leave, and nobody can enter. Not even pets,” Dr. Buchholz says.
Another key piece of equipment: masks. Patients should wear a face mask anytime they leave their room, and these excursions should be limited—in other words, bathroom trips only. Anyone entering the room should also wear a mask, and the sick person should likewise mask up for all visitors, regardless of age.
A simple surgical mask is recommended for home use, but given shortages, you can improvise with a scarf tied securely around the face, says Dr. Buchholz. Even hardware-store face masks used for projects like painting or sanding are better than going barefaced. The point is to keep the nose and mouth well-covered, because “if the sick person has a surprising cough or sneeze, you may not be able to turn away fast enough,” he says. Glasses are helpful for keeping spray droplets out of the eyes.
Tying a bandanna over the face outlaw-style isn’t ideal because it will gape at the chin, says Audrey Chun, a doctor in geriatrics and palliative medicine at Mount Sinai Hospital in New York City. “You want the mask to catch the particles from a sneeze, so it’s not spewing out the sides or the bottom,” she says.
You’ll also need gloves—rubber or latex—when you enter the sickroom or when you clean. Stock up on cleaning supplies, because everything the sick person touches—like cutlery, doorknobs or the bathroom sink—must be cleaned. You can make a DIY bleach preparation by diluting five tablespoons of bleach per gallon of water. Regular hand soap is crucial, too.
“I cannot emphasize enough the importance of hand hygiene: washing your hands with warm, soapy water and wiping down surfaces that have been touched. We know this works,” Dr. Chun says. She recommends a nail brush to scrub under fingernails.
If the bathroom is shared, sick people should use disposable paper towels instead of a shared hand towel, Dr. Buchholz says. Keep their bath towels separate from everyone else’s. And healthy family members should remove their toiletries from the shared space. “You don’t want toothbrushes to be anywhere near each other,” he says.
MEDICINE
Medical supplies: cough drops; over-the-counter cold medicines; pulse oximeter and batteries (there is a pulse-oximeter app available for the iPhone, but none of the doctors we spoke to recommended it); saline nasal spray; thermometer; Tylenol/acetaminophen (children’s or infant’s versions if applicable).
Anyone who falls ill should keep in contact with their doctor and let them know if symptoms worsen. To that end, a thermometer is helpful. Since Covid-19 can affect breathing, several doctors also recommended obtaining an at-home pulse oximeter: a device that clips onto the finger and measures heart rate and blood oxygen levels, which are important indicators of how well the lungs are functioning, says Andra Blomkalns, chair of emergency medicine at Stanford School of Medicine. “I ordered 600 of them to send home with patients, and I’m glad I did.” Oximeters are sold over the counter at pharmacies and retailers.
“For a really sick person who’s not sick enough to be admitted to the hospital but they’re on the edge, having an oximeter can be incredibly reassuring,” Dr. Buchholz says.
Have your regular cold medicines on hand and Tylenol or acetaminophen. If the patient is under 18, make sure you have children’s or infant’s versions.
“For the vast majority of kids, you can just stick to the items you would normally use for influenza or other respiratory ailments,” says Danielle Zerr, chief of pediatric infectious diseases at Seattle Children’s Hospital. It is difficult to get children to wear a face mask, so the caregiver must wear one at all times when interacting with the sick child, she says. The child’s Covid-19 symptoms may be mild, but “it’s the same virus, and it’ll be much worse in an adult,” she says.
For a dry cough, throat lozenges can be helpful, as long as the child is old enough not to choke on them. For younger children, “if they have throat pain, a little bit of warm tea with honey is a nice way to go,” Dr. Zerr says.
FOOD AND DRINK
Nutrition supplies: chicken soup; daily multivitamin and vitamin C tablets; electrolyte-replacement drinks (if using sports drinks, cut in half with water); fresh ginger, lemons, dill, fresh or dried oregano; high-calorie, nutrient-rich foods like avocados; honey for throat soothing; pectin-rich foods like bananas and apples.
As with any flulike virus, it is important that the patient drink plenty of fluids. Occasionally, Covid-19 can cause gastrointestinal distress and diarrhea, and replenishing fluids in those cases is especially important, as dehydration can worsen a fever, Dr. Blomkalns says. Electrolyte-replacement drinks are recommended, but popular sports drinks like Gatorade tend to have high amounts of sugar, so they should be cut in half with water for both children and adults, she says.
Another reason to cut sports drinks with water is that sugar can make diarrhea worse. Sugar-free beverages with artificial sweetener aren’t recommended either, because that, too, can worsen gastrointestinal problems, Dr. Chun says. She recommends pectin-rich foods like bananas and apples to ease symptoms of diarrhea.
Some patients tend to lose their appetite when sick, especially children, so Dr. Zerr recommends having on hand comforting, high-calorie but nutrient-dense foods like apple sauce and avocados.
A couple of doctors recommended a daily multivitamin and vitamin C tablets. “And never underestimate the power of chicken soup,” says Mark Hyman, head of innovation at the Cleveland Clinic Center for Functional Medicine. “Protein is very important when fighting viral illnesses.”
He recommends adding dill, oregano and ginger to soups for their antiviral properties. One of Dr. Hyman’s favorite home remedies is his “cold-buster tea”: a 2-inch chunk of fresh ginger root, sliced thin, boiled in a pot of water for several minutes. Add fresh lemon juice, honey and cayenne pepper. Steep for five minutes. “It becomes this spicy, sweet and tangy thing,” he says. “It’s great.”
Ms. Potkewitz is a writer in New York. She can be reached at [email protected]. Click Here to view the original article on WSJ.com.
